This study aims to provide crucial in vivo pharmacokinetic parameters, essential for optimizing therapeutic strategies and understanding the drug’s efficacy and safety in this sensitive population.
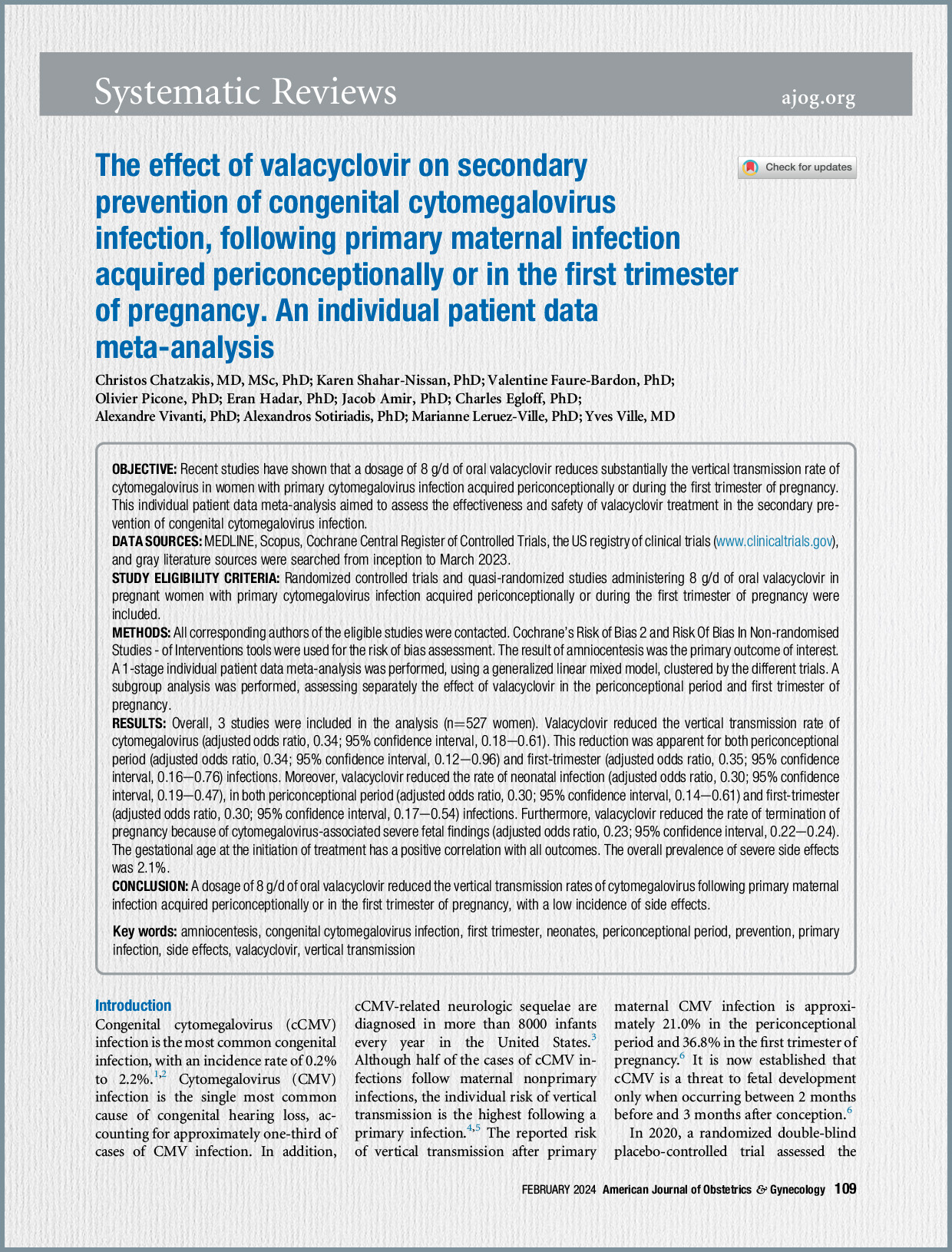
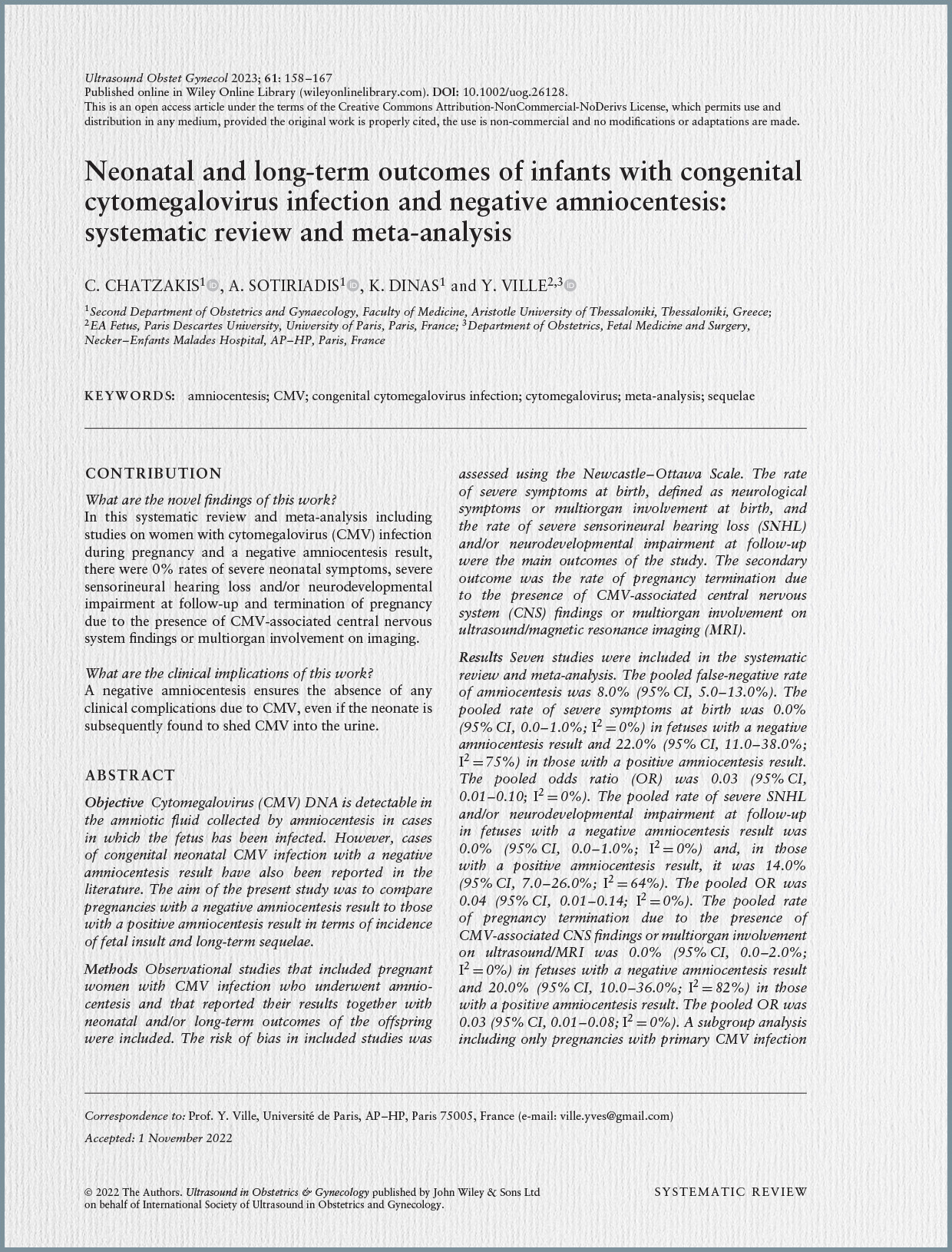
Background and Rationale for Valacyclovir Use: Congenital CMV infection remains the most common congenital infection and the leading non-genetic cause of sensorineural hearing loss (SNHL) [Summary of Chatzakis 2023, 10, 33]. It can lead to severe neurological defects and other long-term sequelae in affected infants [Summary of Chatzakis 2023]. The vertical transmission rate after a primary maternal CMV infection (CMV-MPI) can be substantial, around 40% [Summary of Chatzakis 2023]. Therefore, interventions aimed at preventing this transmission are of significant clinical interest.
Valacyclovir, an antiviral agent, has been investigated for its potential to prevent vertical transmission following CMV-MPI. The specific dosage of 8 grams per day (8 g/day), often administered in two 4-gram doses or four 2-gram doses, was initially chosen due to its demonstrated effectiveness in preventing CMV disease in CMV-negative renal transplant patients receiving CMV-positive grafts. The hypothesis supporting its use in pregnancy considers the fetus as a host and the mother as a graft, aiming to reduce maternal viral load, prevent vertical transmission, and mitigate fetal CMV infection and disease. Prior research indicated that valacyclovir 8 g/day could reduce transplacental passage of the virus by 70%. However, comprehensive pharmacokinetic data for this high dose specifically within pregnancy have been lacking.
Challenges and Knowledge Gaps Highlighted by Other Sources: The broader context of CMV management, as described by other sources, underscores the importance of this PK study. For instance, the French Haut Conseil de la Santé Publique (HCSP) report from December 2023 explicitly does not recommend universal CMV screening during pregnancy. A key reason cited is the unknown efficacy and risks of prolonged high-dose valacyclovir treatment on fetal outcomes. The HCSP report highlights several methodological weaknesses in the pivotal randomized trial by Shahar-Nissan et al. (2020), which suggested an efficacy of valacyclovir on vertical transmission. Specifically, the HCSP noted that the main outcome of that study (vertical transmission) was not the most pertinent, as the critical concern is the prevention of severe neuro-sensory sequelae in the child, for which data are still missing. Moreover, the HCSP raised concerns about the maternal safety profile of the 8 g/day dose, noting reports of acute kidney injury (AKI), particularly with a 4g/12h regimen. This pharmacokinetic study directly addresses the need for a better understanding of the drug’s exposure, a foundational element required to confidently evaluate its benefit-risk ratio.
Objectives of the Current Study: The primary objective of this population PK study was to quantify maternal and fetal valacyclovir exposure by establishing comprehensive pharmacokinetic parameters in vivo. By detailing how the drug behaves within the maternal and fetal compartments, the study aims to provide a better understanding of the therapy’s mechanism and to inform the refinement of optimal therapeutic management for maternal CMV seroconversions and fetal CMV infections during pregnancy.
Methodology: This was a population pharmacokinetic (popPK) study assessing the use of valacyclovir 8 g/day in CMV-infected pregnant women. The study participants were pregnant women with confirmed CMV-MPI. Maternal seroconversion was biologically verified at a national reference center using IgG, IgM, and IgG avidity testing. The timing of maternal infection was estimated using a standardized algorithm, defining periconceptional (approximately 3 months before conception) and first trimester (0-14 weeks of amenorrhoea) periods.
All participants received oral valacyclovir at a dose of 8 g/day. The administration regimen varied: 81.5% of patients received 2g every 6 hours (2g/6h), while 18.5% received 4g every 12 hours (4g/12h). Amniocentesis was performed at a median gestational age (GA) of 17.4 weeks (range 16.7–23.6 weeks), following a median treatment duration of 35 days (range 7–90 days). Fetal infection was assessed by CMV PCR on amniotic fluid samples. Notably, all ultrasound findings related to the placenta, amniotic fluid, and fetal weight (all eutrophic) were reported as normal for the study cohort.
Key Findings:
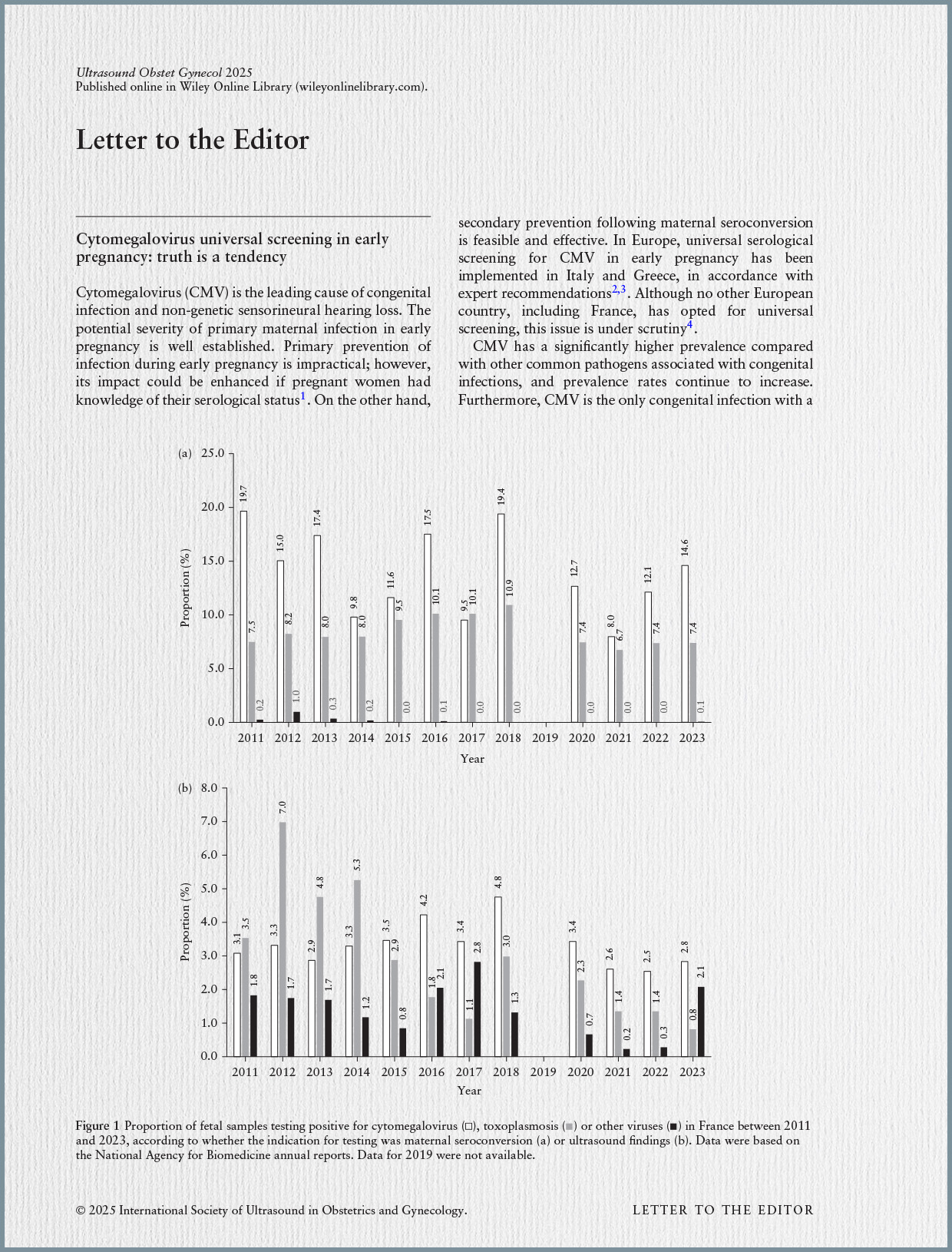
- Vertical Transmission Rate: Despite maternal valacyclovir treatment, 12 out of 122 (9.8%) amniotic fluid samples were CMV PCR positive, indicating that vertical transmission had occurred. This rate is notable when compared to the 8.0% false-negative amniocentesis rate previously reported in cases where neonatal CMV infection occurred without severe outcomes [620, Summary of Chatzakis 2023].
- Maternal Pharmacokinetic Parameters (Median and Range):
- Area Under the Curve (AUCmat, 0–24 h): 570.2 µmol.h/L (range: 297.6–1282.4).
- Minimum Concentration (Cminmat): 9.6 µmol/L (range: 0.3–38.6).
- Maximum Concentration (Cmaxmat): 40.7 µmol/L (range: 27.1–87.9).
- Amniotic Fluid Pharmacokinetic Parameters (Median and Range):
- Area Under the Curve (AUCAF, 0–24 h): 562.4 µmol.h/L (range: 293.6–1229.2).
- Minimum Concentration (CminAF): 21.2 µmol/L (range: 9.3–48.8).
- Maximum Concentration (CmaxAF): 25.4 µmol/L (range: 13.4–52.8).
- Comparison Between Transmitters and Non-Transmitters: The study did not find a clear difference in median maternal or fetal PK parameters (AUC, Cmin, Cmax) between pregnant women who transmitted the virus to their fetuses and those who did not. This suggests that the achieved drug exposure levels were similar irrespective of transmission outcome within the cohort.
- Fetal Ultrasound Findings: All placental, amniotic fluid, and fetal weight assessments via ultrasound were reported as normal for the entire cohort. This finding, while not a direct PK result, provides reassuring clinical context regarding the absence of overt fetal insults in the studied population treated with valacyclovir.
Discussion and Implications: This study represents a significant contribution by providing the first in vivo quantification of valacyclovir PK parameters in both maternal and fetal compartments during pregnancy for the 8 g/day dose. This data is invaluable for understanding the systemic exposure of the drug in this specific population.
The observed 9.8% vertical transmission rate despite treatment indicates that valacyclovir, at the current dosing, does not completely eliminate the risk of transmission. This finding is particularly important when juxtaposed with previous research indicating that a negative amniocentesis (even if a false negative for transmission) correlates with a 0% rate of severe neonatal symptoms or long-term sequelae. While this PK study does not evaluate the clinical outcomes of these 9.8% transmissions, it emphasizes that even with therapeutic levels, some transmissions can still occur.
The finding that PK parameters did not significantly differ between transmitters and non-transmitters suggests that simply achieving a certain drug concentration within the measured ranges may not be the sole determinant of transmission prevention. This implies that other factors, such as viral load dynamics, maternal immune response, the exact timing of infection relative to treatment initiation, or variations in viral strains, might play a crucial role in vertical transmission. This insight is critical for refining future treatment protocols, potentially leading to more personalized or adaptive dosing strategies.
Furthermore, the data from this study provides a concrete basis for addressing the concerns raised by health authorities like the HCSP regarding the safety and efficacy of high-dose valacyclovir. While this PK study itself did not report on maternal adverse events, other sources have highlighted the risk of acute kidney injury (AKI) with the 8 g/day dose, particularly when administered in two large doses. The detailed PK data from this study will be essential for future modeling and clinical trials to determine optimal dosing regimens that maximize efficacy while minimizing maternal and fetal risks. The observation of normal ultrasound findings in the cohort provides some preliminary reassurance regarding the lack of immediate detectable fetal harm, although long-term follow-up of exposed children, as emphasized by the HCSP, remains critical.
Conclusion: This pharmacokinetic study successfully established maternal and fetal valacyclovir exposure parameters at the 8 g/day dose in pregnant women with primary CMV infection. These novel in vivo data are fundamental for a deeper understanding of valacyclovir’s pharmacological behavior during pregnancy. The findings suggest that while high concentrations are achieved in both maternal and amniotic fluid compartments, the measured drug exposure alone does not fully differentiate between cases of vertical transmission and non-transmission. This study’s contribution is vital for informing future clinical trials and refining optimal therapeutic management strategies for congenital CMV, aiming to balance efficacy in preventing transmission and severe sequelae with the safety of the pregnant mother and fetus, addressing a key need identified by international health bodies.