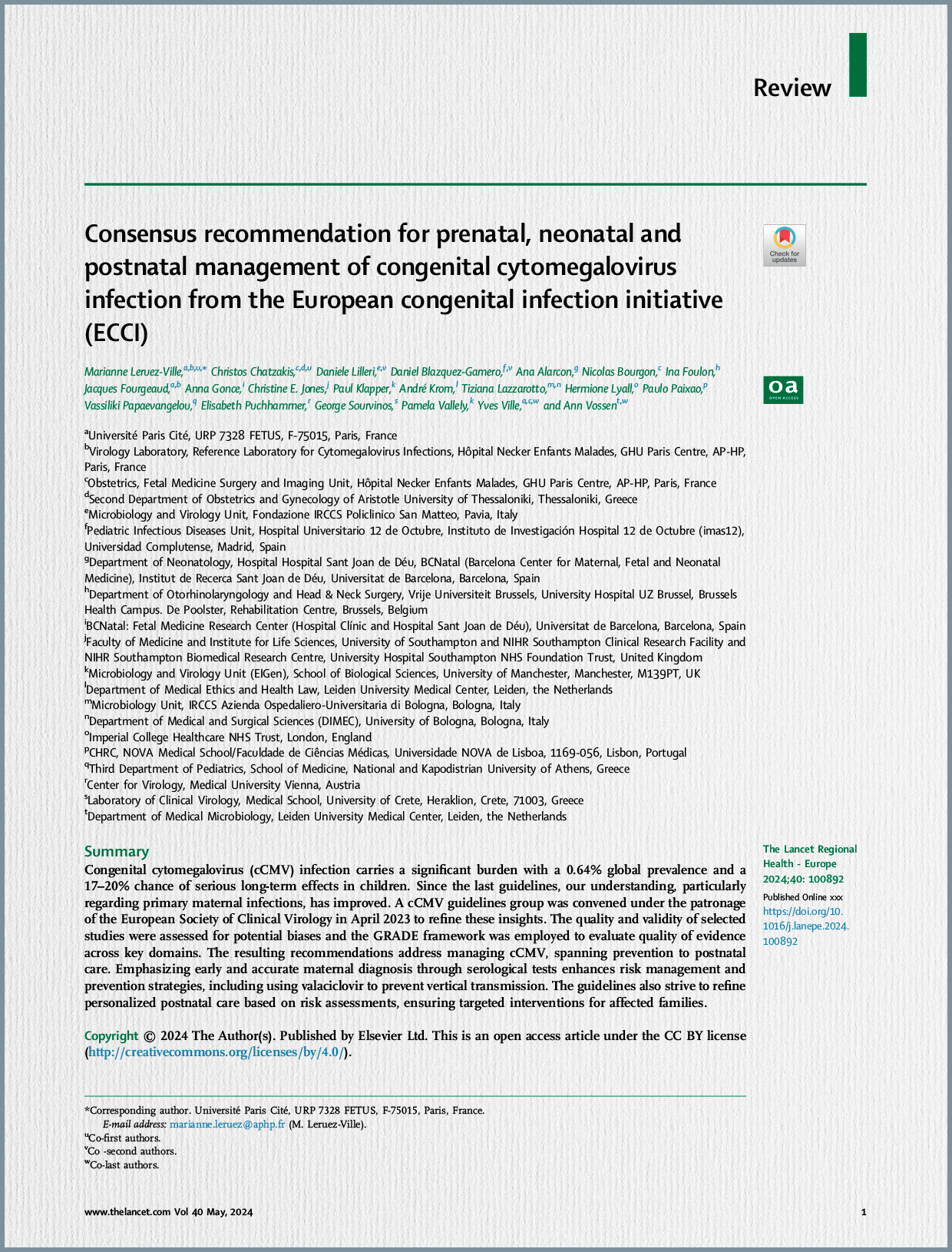
A critical aspect emphasized is that sequelae are primarily limited to cases where maternal infection occurred before 14 weeks of gestation. Despite advances in prenatal assessment using ultrasound and MRI, predicting neonatal status, especially in cases without overt severe cerebral features, remains challenging, underscoring the need for new prognostic biomarkers in amniotic fluid.
Background and Rationale: cCMV is a leading non-genetic cause of sensorineural hearing loss (SNHL) and a major contributor to neurological damage. Approximately 30% of infected newborns are symptomatic at birth, with 10–15% experiencing SNHL and vestibulitis, and 10–25% suffering more severe neurological damage, including intellectual disability or developmental delay. The immunobiology underlying cCMV infection is poorly understood. The study posits that cytokines, which are crucial mediators in innate immunity and immune control of cCMV, could serve as important biomarkers, particularly those transported within or on the surface of extracellular vesicles (EV). A previous study had already indicated elevated levels of interferon gamma-induced protein 10 (IP-10) in the amniotic fluid of infected fetuses.
Study Objectives: The primary objective of this study was to comprehensively investigate the concentrations and profiles of intra-amniotic cytokines, including their soluble, surface-associated, and internal (extracellular vesicle-associated) fractions, in cCMV infection. The goal was to correlate these cytokine profiles with the severity of the infection at birth, thereby identifying potential candidate biomarkers for prognosis.
Methodology: The study was conducted at the Fetal Medicine Unit at Necker Hospital in Paris, enrolling 80 pairs of women and fetuses/newborns between December 2011 and December 2017. This included 40 infected fetuses, whose mothers had primary CMV infection diagnosed within two months prior to conception or in the first trimester of pregnancy, and 40 non-infected, euploid controls, matched for fetal gender and gestational age at amniocentesis. Women with immune disorders or treatments affecting immunity were excluded.
Diagnosis and Classification:
- Maternal Primary Infection (MPI): Timing was determined using an in-house algorithm based on CMV IgG and IgM antibody concentrations and IgG avidity.
- Fetal Infection: Defined by a positive CMV DNA PCR on amniotic fluid (AF) samples. Amniocentesis was performed after 17 weeks of gestation and at least 8 weeks following MPI to ensure optimal diagnostic accuracy.
- Neonatal Infection: Confirmed at birth by CMV DNA PCR on neonatal blood, urine, and saliva. All virological tests were performed by an expert virology laboratory.
- Newborn Classification: Infected newborns were classified as symptomatic if they had at least one abnormal neonatal feature, or if they were deceased fetuses due to severe brain lesions or spontaneous intrauterine fetal death. Symptomatic cases were further divided into “non-severe” and “severe” subgroups. Asymptomatic newborns presented with no growth restriction, no abnormal clinical features, no biological abnormalities (like thrombocytopenia or liver enzyme elevation), and no abnormalities in ophthalmologic or audiologic assessments, or on transcranial ultrasound (TUS). Fetuses with only isolated minor cerebral features (e.g., subependymal cysts or lenticulostriate vasculopathy calcifications) were considered asymptomatic. Severe symptomatic fetuses were those with at least one severe cerebral feature such as cortical abnormalities, significant ventriculomegaly (>15 mm), or microcephaly. Postmortem examinations confirmed severe infection in lethal cases.
Cytokine Analysis: Amniotic fluid samples were stored and processed to separate different fractions: a “soluble fraction” from the supernatant, and “surface” and “internal” (luminal content) fractions from extracellular vesicles (EVs). The concentrations of 38 distinct cytokines were quantified using a Luminex immunoassay. Statistical analysis included filtering out proteins with insufficient non-zero values (77 of 114 remained) and then performing univariate and multivariate analyses to determine associations with infection and severity, with Bonferroni correction for multiple comparisons.
Key Findings:
- Cohort Characteristics: The study included 40 infected fetuses (9 asymptomatic, 31 symptomatic – 13 non-severe, 18 severe) and 40 controls, with similar clinical characteristics between groups.
- Cytokines Associated with Fetal Infection: Univariate analysis revealed a nominally significant increase in six proteins in the amniotic fluid of cCMV infected fetuses compared to controls. These included primarily soluble cytokines such as IP-10, IL-18, ITAC, and TRAIL. Notably, EV-associated IP-10 (both internal and surface-bound) was also significantly elevated. IP-10 was particularly robust, reaching the stringent Bonferroni-corrected p-value threshold for both infection and severity (p < 0.0003).
- Cytokines Associated with Symptomatic Status at Birth:
- Twelve proteins showed a significant correlation with symptomatic status at birth.
- These included four soluble proteins: IP-10, IL-18, TRAIL, and CRP.
- Eight EV-associated proteins, predominantly within the EVs, were also linked: IP-10, IL-6, MCP1, MIG, and RANTES.
- Five cytokines previously associated with fetal infection (soluble, surface, or internal IP-10, soluble IL-18, and soluble TRAIL) were also found to be related to symptomatic outcome.
- A distinct pattern of increased levels of six specific mediators (soluble IL-18, soluble TRAIL, soluble CRP, surface TRAIL, internal MIG, and internal RANTES) was identified as characteristic of severe symptomatic infection.
- Importantly, fetal thrombocytopenia was also significantly associated with severe fetal infection (p < 0.001).
- In contrast, amniotic fluid CMV viral load and fetal liver tests were not found to be associated with fetal symptoms in this cohort.
- Prediction Analysis: The study demonstrated a strong potential for using cytokine profiles to predict both fetal infection and its severity. A model based on five principal components derived from all proteins showed an average AUC (area under the ROC curve) of 0.72 for predicting fetal infection (p = 0.037). For predicting severity, models based on soluble proteins and all proteins combined performed best, explaining up to 41% of the total variance.
Discussion and Conclusion: The findings of this study significantly enhance the understanding of the immunopathological processes in cCMV infection by highlighting changes in the amniotic fluid’s immunological signature. The increase in pro-inflammatory mediators (IP-10, IL-18, ITAC, and TRAIL) in cases of cCMV infection suggests a robust immune response within the intrauterine environment. The identification of distinct cytokine patterns linked to symptomatic status, and particularly severe infection, holds promise for developing new prognostic biomarkers. The confirmation that CRP is associated with severe fetal infection aligns with previous proteomic analyses.
The study’s strengths include its relatively large cohort size and the comprehensive investigation of cytokines across different fractions, including those associated with extracellular vesicles. The exploration of EV-associated cytokines is particularly novel, as EVs are increasingly recognized for their role in intercellular communication and as carriers of biomarkers in biological fluids, including amniotic fluid. Acknowledged limitations include the unbalanced ratio of cytokines to cases and potential sensitivity limitations of the ELISA method for detecting ultra-low concentrations of EV cytokines, suggesting that newer technologies like SiMoA might offer further insights.
In conclusion, the study firmly establishes that cCMV infection and its severity are associated with differential cytokine expression in amniotic fluid at mid-gestation. These proteins, predominantly soluble, emerge as promising candidate biomarkers for assessing the severity of fetal infection diagnosed by CMV-PCR, potentially improving prenatal counseling and intervention strategies.