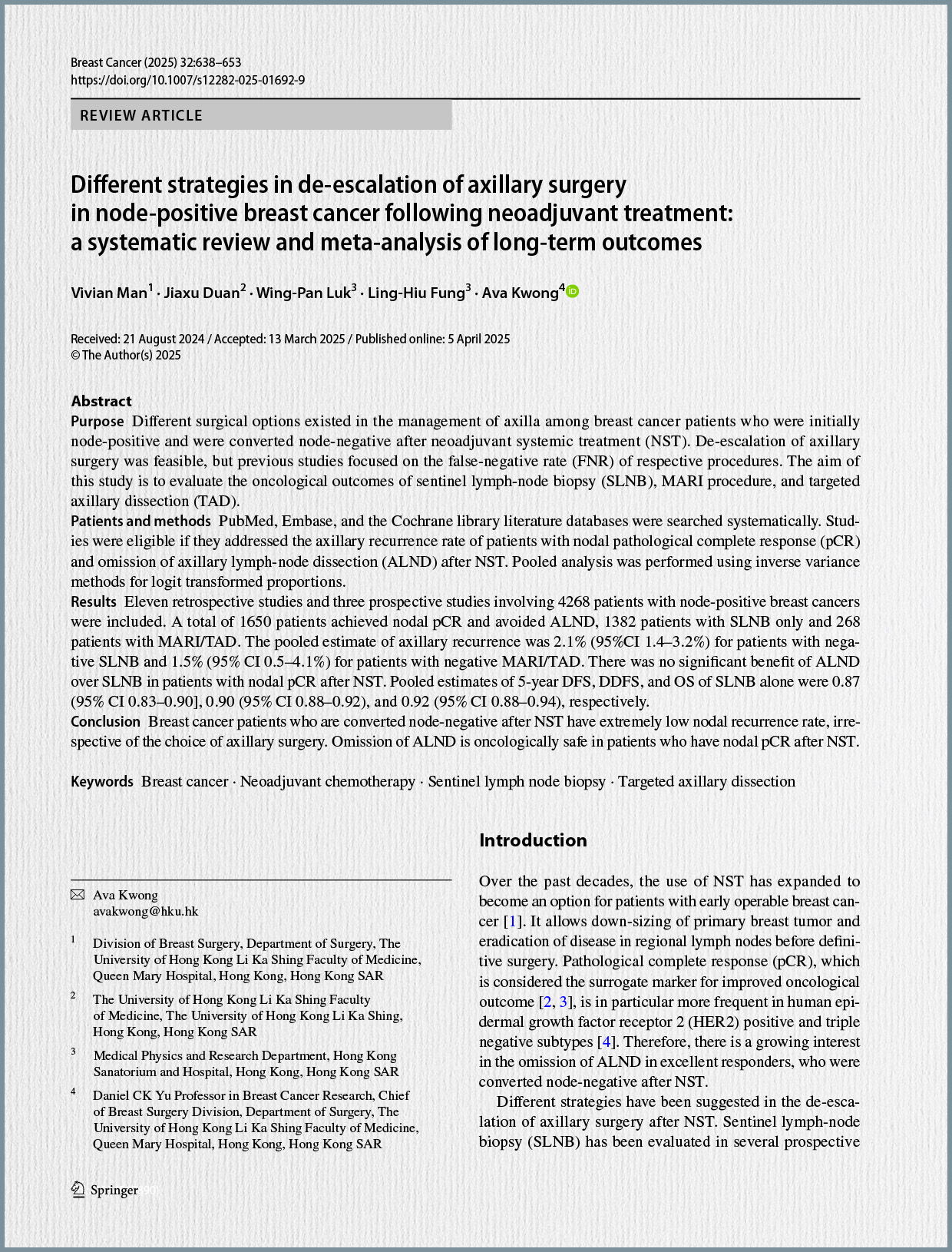
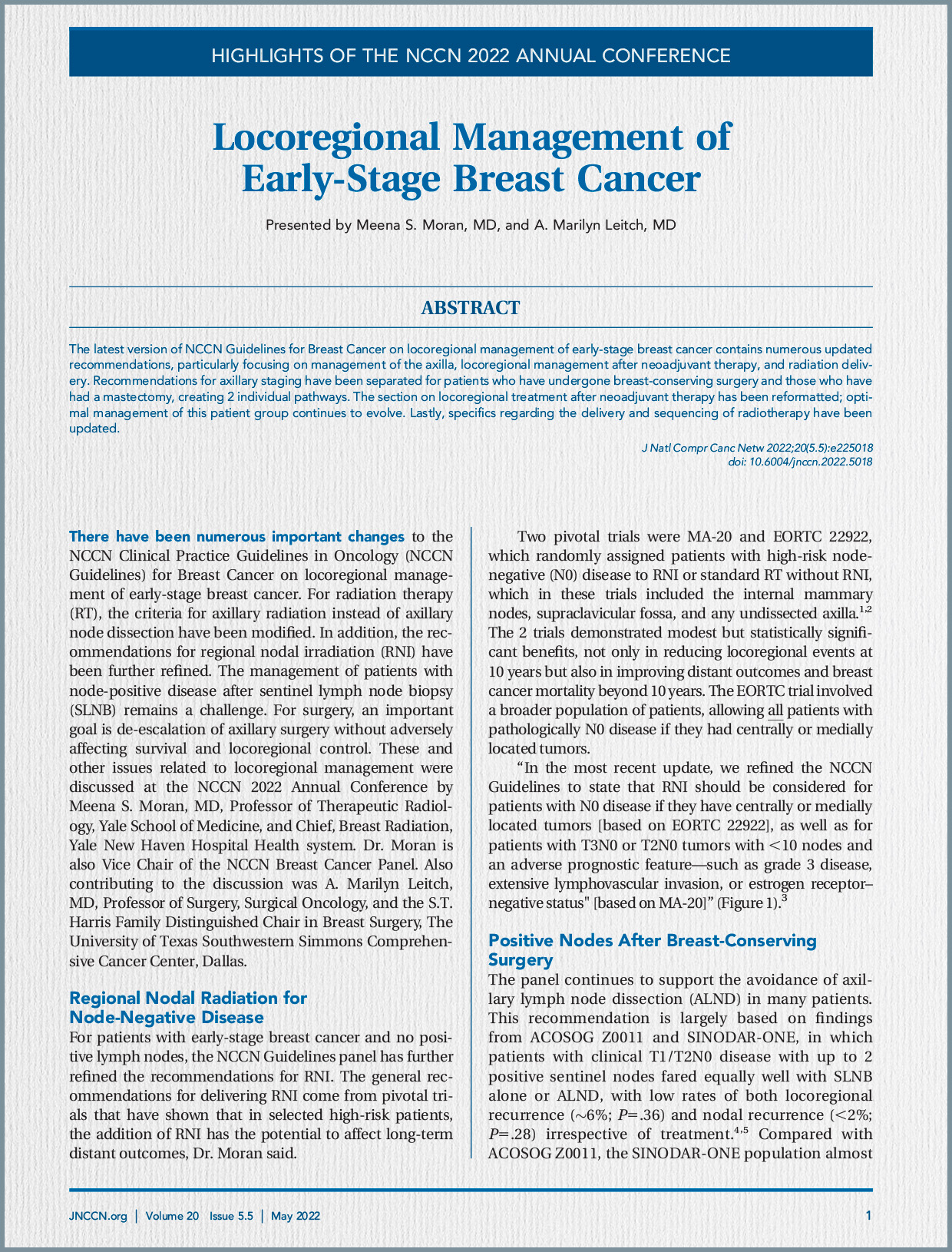
Background and Evolution of Axillary Management
Historically, systematic axillary lymphadenectomy (ALND) was the standard of care for staging and treating breast cancer, based on the understanding that breast cancer spread primarily via the lymphatic system. However, from the 1990s, ALND has been progressively replaced by sentinel lymph node biopsy (SNB). SNB aimed to gain knowledge about the axillary lymph node status without removing the entire axillary basin, particularly in patients without axillary metastases. This shift was driven by the significant morbidity associated with ALND, including lymphedema, nerve damage, reduced shoulder and arm mobility, and chronic pain.
Further de-escalation efforts have challenged the necessity of performing SNB in all invasive breast cancers and the imperative to carry out ALND in all patients with SNB involvement. Recent advancements in understanding breast cancer biology and the advent of targeted therapies have paved the way for further de-escalation of axillary interventions, especially for patients with minimal or no nodal disease.
Neoadjuvant systemic treatments (NST), also known as NAT, have increasingly been utilized, particularly for triple-negative or HER2-positive breast cancer. One of the main purposes of NAT is to downstage the disease in both the breast and axillary lymph nodes, aiming to reduce the extent of subsequent surgery and enable more personalized treatment. A particular area of interest is patients who present with metastatic lymph nodes before NAT but achieve a node-negative status at the time of surgery, known as nodal pathological complete response (pCR). This exceptional response rate, especially in HER2-positive breast cancer with dual HER2 blockade, prompts the question of whether axillary surgery can be entirely omitted in selected subgroups.
Study Methodology
This was a retrospective cohort study conducted at the Oncology Center Mansoura University in Egypt, including patients diagnosed with HER2-positive breast cancer between March 2022 and September 2023. The study included female patients over 18 years old with histological and radiological proof of non-metastatic invasive HER2-positive breast cancer who received neoadjuvant chemotherapy combined with single or dual HER2 blockade. Patients with DCIS, metastatic disease at diagnosis, locally advanced (T4b+) breast cancer, or those unable to receive anti-HER2 therapy were excluded.
Data collected included patient demographics (age, BMI), imaging details (mammogram, MRI, breast density, tumor focality, size, site, BIRADS score, LN status pre-NAT, LN clipping), pathological information (pre-treatment LN biopsy, tumor type, hormonal receptor status, Ki67, HER2 score, luminal type, number of retrieved/positive LNs), NAT specifics (number of cycles, protocols, anti-HER2 type), tumor response (RCB, Miller–Payne, radiological and pathological LN response), surgery type (breast and LN), and adjuvant treatments.
Chemotherapy protocols typically involved combinations of anthracyclines and taxanes, with most patients receiving dual anti-HER2 blockade (trastuzumab + pertuzumab). Post-NAT, patients underwent re-evaluation with breast and axillary imaging before surgery. Surgical decisions for the breast involved breast-conserving surgery or mastectomy, while for the axilla, SNB or ALND was performed based on axillary response and surgeon’s decision. Statistical analyses, including chi-square tests, Fisher’s exact tests, Mann–Whitney U-tests, and binary logistic regression, were used to identify significant predictors and assess diagnostic accuracy.
Key Findings and Results
The study analyzed data from 139 patients. The median age was 50 years, and two-thirds of patients had HR+/HER2+ disease, while one-third had HR−/HER2+ disease. A large majority (92.8%) of patients initially presented with node-positive or suspicious disease, though only 18.7% had biopsy-confirmed nodal involvement.
Following NAT, 112 patients (80.6%) achieved clinically and radiologically negative axillary lymph nodes (cN0). This high rate of nodal response was further confirmed by pathological evaluation: 112 patients (80.6%) ultimately had pathologically node-negative disease (pCR). This implies a complete pathological axillary response in 79.1% of patients within the study cohort. In the study, all patients treated with SNB alone had node-negative disease pathologically, whereas the ALND group showed a mix of node-negative and node-positive cases.
The study identified several statistically significant factors that predicted a complete nodal response (pathologically negative axillary LNs) after NAT:
- Degree of HER2 Positivity: HER2+ 3 tumors were significantly more likely to achieve nodal pCR compared to HER2+ 2 tumors (p=0.024).
- Type of Anti-HER2 Therapy: Dual HER2 blockade (Trastuzumab + Pertuzumab) was significantly associated with a higher likelihood of nodal pCR (p=0.023).
- Pre-NAT LN Status by Imaging: All patients who had radiologically negative LNs before NAT were found to be pathologically negative after NAT.
- Post-NAT LN Status by Imaging: Critically, all 112 patients who showed clinically and radiologically negative axillary LNs after NAT were confirmed to have pathologically negative LNs. This demonstrated a 100% negative predictive value and accuracy for post-NAT radiological assessment in this cohort.
- Primary Tumor Radiological Response: All patients whose primary tumor achieved a complete clinical response (cCR) also had nodal pCR (p<0.001).
- Degree of Pathological Tumor Response: All patients with a residual cancer burden (RCB) of 0 or Miller–Payne Grade 5 in the primary tumor also had nodal pCR.
- While not statistically significant, all T1 primary tumors before NAT showed negative LNs after NAT.
In multivariate analysis, HER2 score and the type of target therapy (dual vs. single blockade) were significant independent predictors of pathologically negative axillary LNs. Patients with HER2+ 3 tumors and those who received dual anti-HER2 blockade had 5.1 and 14.4 times higher odds, respectively, of exhibiting pathologically negative axillary LNs.
Discussion and Implications for Clinical Practice
The remarkably high rates of pathological complete axillary response (79.1%) observed in this HER2-positive cohort underscore the potential for further de-escalation of axillary surgery. The study’s findings suggest that specific patient subgroups can be identified who might safely avoid axillary surgical staging due to their excellent response to NAT.
The absolute correlation between clinically/radiologically negative axillary LNs post-NAT and pathologically negative LNs is a significant finding of this study, potentially being the first to report such a high predictive value. This suggests that for HER2-positive patients achieving clinical nodal negativity after NAT, imaging alone might be sufficient to confirm axillary pCR, potentially avoiding SNB altogether. The consistent finding that all patients with a complete clinical response in the primary tumor also achieved nodal pCR further reinforces this concept, aligning with previous research indicating that nodal positivity is exceedingly rare in such cases.
The study’s results are consistent with the established literature regarding the effectiveness of dual anti-HER2 blockade in achieving pCR. The observation that HER2+ 3 tumors are more likely to achieve axillary pCR than HER2+ 2 tumors also aligns with prior studies.
While the study’s findings are promising, it acknowledges several limitations inherent to its retrospective design, such as potential selection bias and heterogeneity in chemotherapy protocols, the number of anti-HER2 cycles received, and the variability in axillary staging procedures among surgeons. However, its strengths include the use of prospectively maintained data, a reasonable sample size, and the reflection of real-world clinical practice.
Conclusion
In conclusion, this study strongly suggests that axillary staging may be omitted in HER2-positive breast cancer patients who demonstrate clinically node-negative disease after neoadjuvant chemotherapy combined with dual anti-HER2 therapy. This holds particularly true for patients with:
- Early tumors (e.g., cT1-2N0).
- Strong HER2+ disease (HER2+ 3 expression).
- Clinically negative lymph nodes before NAT.
- Primary tumors that achieve a complete clinical response.
The study proposes that, at a minimum, patients with cT1-2N0 tumors and breast cCR are strong candidates for the omission of axillary staging. These findings advocate for a highly personalized approach to axillary management, aiming to reduce surgical morbidity while maintaining excellent oncological control. Nevertheless, the authors emphasize the critical need for further multicenter, prospective, randomized controlled trials to validate these findings and evaluate nodal recurrence rates in these carefully selected patient populations when axillary staging is omitted.